|
|
||||||||||||||
|
Neulasta (Pegfilgrastim) |
||||||||||||||
| Contents and links: What are white cells | Chemotherapy & whites cells | Neulasta studies | Neupogen | Self injection | Preventing infection | Diet & chemotherapy | Exercise & chemotherapy | Lifestyle & chemotherapy | | ||||||||||||||
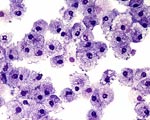
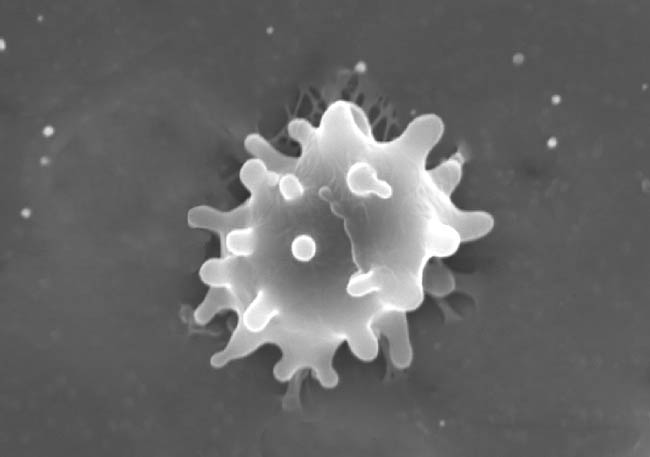
For more detailed information please refer to the product information within the packet or go to the international website. What are white cells? Blood contains three main elements. The red cells which carry oxygen around the body from the lungs, platelets which stop us bleeding when we are cut, and white cells which help our immunity and protect us from infection. There are a number of different types of white cells but one of the most important types, are called neutrophils or granulocytes. These protect us from bacteria, which are the most likely source of infection during chemotherapy.
Sometimes too many white cells are killed and patients become susceptible to infection which can to be serious. This is most likely to happen in the middle week between cycles. If, during chemotherapy, you experience shivering or shaking attacks of fever or feel hot or unwell check your temperature. If it is raised, telephone the Hospital immediately and they will advise you. Do not take Paracetamol or Aspirin as this will bring your temperature down and mask the signs of infection. How does Neulasta work? Neulasta is similar to a naturally occurring protein which stimulates the colonies of white stem cells within the bone marrow causing the level of neutrophils in the blood to rise (Granulocyte Colony Stimulating Factor - GCSF). Increasing the levels of neutrophils in the blood stream reduces the risk and severity of infection. Several well conducted international studies, have proven the effectiveness of Neulasta over no medication at all or the previously commonly used white cell booster Neupogen. When is Neulasta used? Neulasta is used to support chemotherapy to boost the white cell count. Neulasta is not often used at the start of the first cycle of chemotherapy as in most cases it is not necessary (primary prophylaxis). The exception is "high dose" chemotherapy or when chemotherapy is given to people with a higher risk of neutropenia (e.g. the elderly or those who had previous courses of chemotherapy). Sometimes during conventional chemotherapy too many white cells are killed and the patient develops an infection which can be serious. Neulasta is sometimes used, as well as antibiotics, to treat the infection. Firstly, If the white cells (neutrophils) will not or are unlikely to recover by the time the next chemotherapy is due, your Oncologist has three choices:
By giving Neulasta, the chances of neutrophil recovery are increased. This would allow scheduled chemotherapy to be given as planned and prevent unnecessary chemotherapy delays and dose reductions. How should Neulasta be given? Neulasta is given as an injection under the skin (subcutaneous), the usual dose is one 6mg of pegfilgrastim in a pre-filled syringe. The ways in which it is given vary from doctor to doctor and department to department. The most common way is approximately 24 hours after the last dose of chemotherapy. Some patients learn to inject themselves (see tips on how to inject yourself) but in others, your chemotherapy nurse will arrange a district nurse to give it. Possible side effects Neulasta is generally well tolerated and it is often difficult to separate the mild side effects from those caused by the chemotherapy. Even so, occasional side effects can occur and these are mentioned below. It is rarely possible to develop side effects not mentioned here.
These last two symptoms are caused by a mild allergic-like reaction. They can usually be corrected next time by a small dose of oral steroids or antihistamines taken just before your Neulasta injection.
|
||||||||||||||