|
|
||||||||||||||||||||||||||||||||
|
Bone health |
|
|||||||||||||||||||||||||||||||
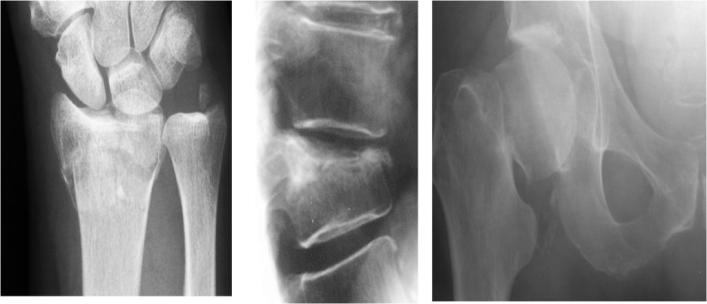
As we get older the bones tend to loose some density but many treatments for cancer can accelerate this process leading to a deficiency of the amount of protein and calcium in the bone (the bone density). This may range from a mild reduction in the calcium density, measured on a bone density scan, to a moderate reduction called osteopenia through to a significant bone mineralisation loss with its associated risks of collapsed vertebrae and fractures (osteoporosis seen in the adjacent picture). Factors which increase the risk of bone loss:
Lifestyle factors which help to maintain healthy bones: Exercise: The bone is not a solid lump of calcium but a dynamic organ constantly re-moulding itself. As a result bone is strongly influenced by environmental and lifestyle factors and of these exercise is the most prominent. Put a man in space, for example and within 6 weeks he has osteopenia as there is no weight baring stimulus to the bone. In a less dramatic but similar way developing a sedentary lifestyle will result in bone thinning. Fortunately weight bar ring exercises will do the opposite. It sends signals to the cells in the bone to lay down more calcium and especially combined with an adequate diet will prevent bone loss or increase it. Exercise, therefore is defense against bone loss and the exercise section describes ways to increase weight baring exercises in a fun controlled and regular way.Dietary calcium is also important and it is not just found in dairy products such as milk, yogurt and cheese but in a wide range of less fatty foods such as sardines, broccoli, almonds and salmon. Vitamin D serves several important functions in relation to calcium metabolism and is vital for the development of healthy bones. It helps to increase calcium absorption from the gastrointestinal system and kidney and thereby make it available to body tissues and the blood. It also functions to aide with the deposition of calcium to bone. The body’s main source of vitamin D arises from the manufacture of this vitamin in the skin on exposure to sunlight. Research has found many people are deficient in vitamin D due to more time being spent indoors. Only 10 – 15 minutes of exposure to outdoor sun is necessary for the production of vitamin D (see sense in the sun). Dietary sources of vitamin D are limited but sources arise often from foods fortified (boosted) with vitamin D such as milk, soya drinks and cereals. It is also found naturally in liver, fish (tuna, salmon, sardines, herring and mackerel) and egg yolk. Plant based protein: A number of studies have demonstrated the importance of plant based proteins to help maintain bone density. In fact, individuals who consume their proteins from plant rather than animal sources actually have better bone density. These include lentils, soya, beans, pulses particularly quinoa. Other lifestyle factors. The National osteoporosis risk assessment study identified several lifestyle factors that correlated with an increased risk of bone loss. These included being underweight (BMI < 18.5kg/m2), smoking (see quit smoking tips), drinking excess caffeine (>4 cups of coffee/day)
How to measure bone density
During a DEXA scan, you will be asked to lie on your back on a couch and to keep still while the scan is being taken. The scan usually takes between 10 and 20 minutes, depending on which part of your body is being examined, and whether a central or peripheral scanner is being used. There are no injections. In order to check for osteoporosis, the doctor commonly scans the lower back bones (vertebrae) and hips. The forearm may also be scanned, because it has a different level of calcium content from other body parts. No preparation for the test is required and, depending on which part of your body is being scanned, you may be able to remain fully dressed, in clothes without metal fastenings. It is a painless procedure and you can go straight home afterwards. Most scans produce a T score and a Z score referring to the bone density in a number of areas of the body. Usually this includes the spine and hips but can often include the wrist and ankle. A T score of zero is normal. Less than zero means the bone density is impaired and your bone density may need some lifestyle or medical attention. The table below gives an example of management recommendations for varying T-scores. The Z score is basically a T score but adjusted to the age at the time of the scan
Other issues with bisphosphonates Bisphosphonate prescribing; eg Risedronate 35mg or Aledronate 70mg PO once weekly. Always prescribe a calcium/vitamin D supplement such as Adacal-D Weekly bisphosphonate dosing is effective, better tolerated than daily (avoids daily insult to oesophagus) with better compliance. Dosing instructions are critical and should be reinforced at follow-up visit: take first thing in the morning, follow by drink of water, sit upright for 30 minutes, do not take lying down and do not eat or drink for 30 minutes after taking the tablet. DEXA response to bisphosphonates is virtually universal (failure of response is a sign of non-compliance), so no need to rescan until end of five year course (more valuable to spend time ensuring compliance at each follow up visit). Bisphosphonates are absolutely contraindicated in pregnancy so make sure younger patients are aware of this and taking appropriate precautions, even if apparently menopausal. A 6 month washout period is needed after risedronate if attempting to conceive (which is the same as the recommended tamoxifen washout period). Patients who cannot tolerate oral bisphosphonates and have T scores less than -2.5 should be given monthly pamidronate infusions for five years. Other intravenous preparations as they become licensed may become preferable. Patients who have moderate to severe renal failure should only take Bonefos only under strict supervision. Care should be taken with Bonefos if it is taken with non-steroidal anti-inflammatory drugs. |
||||||||||||||||||||||||||||||||